Abstract
The treatment of relapsed or refractory (R/R) acute myeloid leukemia (AML) has been a challenge for several decades. Despite the widespread use of cytarabine-based chemotherapy and novel targeted agents, the 5-year overall survival (OS) of AML is still only about 30%, and patients mostly die from relapsed AML. Single-cell RNA sequencing (scRNA-seq) has been applied in the study of recurrence and metastasis of solid tumors, but there is still a lack of in-depth exploration of AML. Here, we investigated the transcriptome features of leukemia stem cells (LSCs) in R/R AML, explored their markers and mechanisms of relapse and chemoresistance, and provided potential therapeutic targets for the clinic.
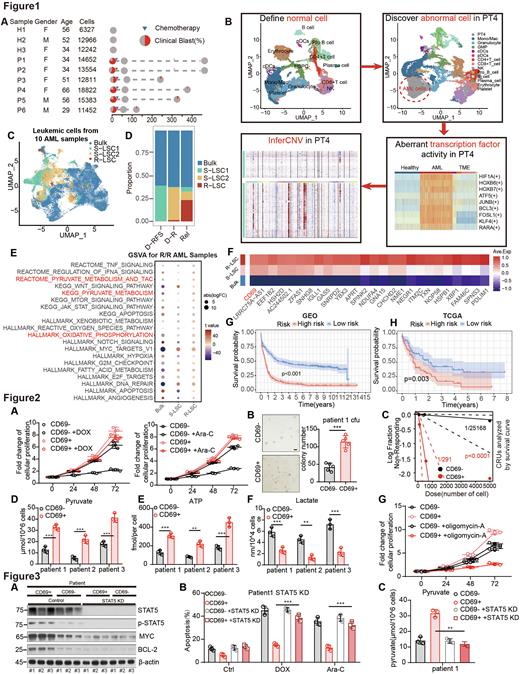
To explore the features of LSCs in R/R AML, we collected 13 bone marrow samples for scRNA-seq, including 8 samples from 4 AML patients at the time of initial diagnosis and their relapse after chemotherapy between 2017 and 2021 (median time to relapse was 333.5 days), 2 samples at initial diagnosis from AML patients with relapse-free survival for three years after chemotherapy, and 3 healthy donors (Figure.1A). Through clustering algorithm, activity analysis of relugons and copy number variation analysis comparing with normal bone marrow samples, we isolated AML cells from normal cells (Figure.1B). Changes of cell number of each cluster and leukemia stemness gene scores were used to define stemness-deficient leukemia cells (Bulk), chemotherapy-sensitive LSCs (S-LSC), and resistant LSCs (R-LSC) (Figure.1C-D). Compared with S-LSCs or Bulk, R-LSCs significantly upregulated the oxidative phosphorylation pathway (Figure.1E). Besides, we found that CD69 was significantly upgraded in R-LSCs, indicating that CD69 may represent a group of leukemic-regenerating cells (LRCs) associated with both leukemic stemness and chemoresistance (Figure.1F) . To investigate the impact of upregulated genes in R-LSC on the clinical prognosis of AML, we explored GEO database and found that the highly expressed genes in R-LSCs including CD69 were associated with a worse clinical prognosis (Figure.1G). TCGA database was used as a validation, and consistent results were obtained (Figure.1H).
To explore the stemness, chemoresistance, and metabolic function of CD69+ LRCs, we sorted CD69- and CD69+ AML cells from patients. Through in vitro chemotherapy, we found that CD69+ AML cells were more resistant to chemotherapy than CD69- AML cells (Figure.2A). By clone formation assay, we found that CD69+ AML had better clonal proliferation ability (Figure.2B). To explore the stemness of CD69+ AML cells, we performed limiting dilution analysis (LDA) in vivo and found that the LSCs ratio of CD69+ AML was 109 times that of CD69- AML (p < 0.0001) (Figure.2C). Next, we explored the metabolic function of CD69+ AML cells and found that CD69+ AML cells had higher levels of pyruvate and ATP metabolism, while lactate metabolism levels were lower than those of CD69- AML cells (Figure.2D-F). After culturing with the ATP synthase inhibitor, the chemosensitivity of CD69+ AML cells was significantly improved (Figure.2G). The above evidence proves that CD69 marks a population of LRCs with high oxidative phosphorylation, stemness and chemoresistance in AML, which is consistent with the scRNA-seq results.
Based on the above conclusions, we further explored the mechanism by which CD69+ LRCs maintain chemoresistance properties. By scRNA-seq analysis, we found that CD69+ LRCs had enhanced activity of STAT5 in the regulatory network (Figure.3A). We found the expression of phospho-STAT5A, MYC and BCL-2 proteins in CD69+ AML cells of patients was significantly higher than that in CD69- AML cells. To explore whether the function of CD69+ LRCs is affected by the JAK3-STAT5 pathway, we knocked down STAT5 in human AML cells. The protein expressions of MYC and BCL-2 were significantly reduced (Figure.3B). The chemosensitivity in vitro was significantly reduced in STAT5 knockdown (KD) (Figure.3C). To explore the effect of STAT5 KD on the metabolism of CD69+ LRCs, we detected metabolic index. We found that CD69+ LRCs with STAT5 KD produced decreased levels of pyruvate (Figure.3D).
In conclusion, CD69 markers LRCs with high oxidative phosphorylation. CD69+ LRCs affect their metabolism and stemness through JAK3-STAT5 activation of downstream MYC and BCL-2. CD69-targeted and STAT5-targeted inhibitors may be candidate strategies for clinical R/R AML treatment.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal